Mohs Surgery is a highly precise and effective technique used to treat most common types of skin cancer, including basal cell carcinoma and squamous cell carcinoma. Performed in stages during a single clinic visit with local numbing, the procedure involves removing thin layers of cancerous tissue and examining them under a microscope in real time until no cancer cells remain where the surgeon is also the pathologist. This method allows dermatologic surgeons to preserve as much healthy skin as possible while ensuring complete cancer removal, making it ideal for delicate or cosmetically sensitive areas like the face. At our clinic, Mohs surgery is performed by our specially trained dermatologic surgeon Dr. Darabi, offering patients the highest cure rates with minimal scarring.
Learn more from the American Society for Mohs Surgery.
(simple surgical removal)
Excision of a Skin Lesion with Local Anesthetic is a common dermatologic procedure used to remove moles, cysts, skin cancers in low risk areas such as the torso and extremities, or other abnormal skin growths, without immediate examination of the removed tissue in the clinic by the surgeon which is the main difference between an excision and Mohs surgery (see above for more information about Mohs surgery).
This procedure is quick, safe, and performed in-office, usually taking 30 minutes.
The skin around the lesion is cleaned thoroughly with an antiseptic solution to minimize the risk of infection.
A small needle is used to inject a local anesthetic (such as lidocaine) around the lesion. This numbs the area so the patient feels no pain during the procedure—just slight pressure or movement.
Once the area is numb, the dermatologist uses a scalpel to surgically remove the lesion, often along with a small margin of normal skin to ensure complete removal. The depth and shape of the excision depend on the type and location of the lesion.
The wound is usually closed with stitches (sutures) to promote healing and minimize scarring. In some cases, deeper stitches are used under the skin in addition to surface stitches for better scar results.
A sterile bandage is applied, and the patient is given instructions for wound care at home, including keeping the area clean, applying ointment (often Vaseline), and changing bandages daily.
Stitches are typically removed in 5–14 days, depending on the location on the body. Usually, the excised tissue is sent for examination by a pathologist and the results are usually available within two weeks.
We can remove certain types of moles using a technique called shave excision or shave removal, which is a quick and minimally invasive in-office procedure. After numbing the area with a local anesthetic, the dermatologist uses a small surgical blade to gently shave the mole down to the level of the surrounding skin. This method is typically used for raised, benign moles that do not require full-thickness removal. The wound is then cleaned and covered with a bandage, and healing usually occurs within a week or two, leaving a flat scar. The removed tissue may be sent to a lab for biopsy to ensure it is non-cancerous.
A cyst can be safely and effectively removed by a dermatologist through a minor in-office surgical procedure. After numbing the area with a local anesthetic, the dermatologist makes a small incision over the cyst and carefully removes the entire sac and its contents to prevent recurrence. If only the contents are drained and the sac is left behind, the cyst is likely to return. The area is then cleaned and closed with stitches if needed, and a bandage is applied. The procedure is quick, and most patients recover with minimal discomfort and scarring. The removed tissue may be sent for pathological analysis.
A shave removal is a quick, in-office procedure used to remove raised skin lesions such as moles, skin tags, or benign growths. After numbing the area with a local anesthetic, the dermatologist uses a small surgical blade to gently shave the lesion flush with the surrounding skin. Stitches are not typically required. After the procedure, the area is cleaned and covered with a bandage.
Aftercare involves daily cleansing with mild soap and water, applying a thin layer of Vaseline, and covering the area with a clean bandage until it heals—usually within 1 to 2 weeks. Patients should avoid picking at the site and protect it from sun exposure to reduce the risk of discoloration. It is normal for the shave wound to have a yellow-white film. This yellow white film is called fibrin and protects the wound and promotes wound healing.
The final scar is generally flat, slightly lighter or darker than the surrounding skin, and tends to fade over time. Most shave removal sites heal with minimal scarring.
At our dermatology clinic, we offer a variety of treatments to help improve the appearance of surgical scars. While some scarring is a natural part of the healing process, several options can help minimize their visibility. Silicone gel sheets or topical silicone products can flatten and soften scars when used consistently early on after the wound has healed over. Laser treatments can reduce redness and improve texture, especially for raised or discolored scars. Microneedling may also be recommended to stimulate collagen and smooth the skin's surface. In some cases, steroid injections can help flatten thick or raised scars such as keloids. Sun protection is essential to prevent scar darkening. Our dermatology providers will assess your scar and create a customized treatment plan to help you achieve the best cosmetic result.
Skin cancer is the most common form of all cancer and includes several types, each with different characteristics and treatment approaches. The three most common types are basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma. BCC and SCC are typically slow-growing and have excellent prognoses when detected early. Melanoma, while less common, is more aggressive and can spread quickly if not treated promptly.
The majority of basal cell cancers are detected early and easily treatable with outpatient procedures such as electrodesiccation and curettage (EDNC), surgical excision or Mohs surgery.
While basal cell carcinoma (BCC) is typically slow-growing and rarely spreads, in rare cases it can become aggressive and invade deeper tissues such as muscle, bone, or nearby structures—especially if left untreated for a long time. Though metastasis is extremely uncommon, advanced BCC can cause significant local damage and disfigurement. At our dermatology clinic, we emphasize early detection and treatment to prevent complications. For aggressive or advanced cases, we offer specialized care including Mohs micrographic surgery, radiation therapy, or if needed referral to medical oncologists for targeted medications such as hedgehog pathway inhibitors. Timely diagnosis ensures the best chance for a successful outcome.
Yes, squamous cell carcinoma (SCC) can become aggressive and spread if not treated promptly. While many cases of SCC are caught early and treated successfully, some tumors—especially those on high-risk areas like the lips, ears, or scalp, or those in immunocompromised patients—can grow quickly, invade surrounding tissues, and even metastasize to lymph nodes or distant organs. Because of this potential for aggressive behavior, it’s important to have SCC evaluated and treated by a dermatologist as soon as possible. Treatment options include surgical excision, Mohs micrographic surgery, radiation therapy, and, in advanced cases, systemic treatments like immunotherapy. Early detection is key to preventing complications and ensuring the best prognosis.
Melanoma is the most serious type of skin cancer, developing from melanocytes—the pigment-producing cells in the skin. It often appears as a new mole or a change in an existing mole, with warning signs including asymmetry, irregular borders, multiple colors, a diameter larger than a pencil eraser, or evolving shape and size. While melanoma is less common than other skin cancers, it can grow quickly and spread to other parts of the body if not caught early. The prognosis for melanoma depends heavily on how early it is diagnosed. When detected in its earliest stages, melanoma is highly treatable with excellent survival rates. However, advanced melanoma that has spread beyond the skin can be life-threatening and requires more aggressive treatment. At our dermatology clinic, we specialize in early detection, skin cancer screenings, biopsies, and personalized treatment plans to ensure the best possible outcomes for our patients.
Melanoma Treatment Options
Treatment for melanoma depends on the stage and depth of the cancer, as well as the patient’s overall health. For early-stage melanomas, surgical excision is the most common and effective treatment, removing the tumor along with a margin of healthy skin. If melanoma has spread to nearby lymph nodes, lymph node biopsy or removal may be necessary. For more advanced or metastatic melanoma, treatment may include immunotherapy (which boosts the body’s immune system to fight cancer), targeted therapy (which attacks specific genetic mutations in melanoma cells), radiation therapy, or chemotherapy in select cases. At our dermatology clinic, we work closely with specialists in oncology to provide comprehensive care and ensure each patient receives a personalized treatment plan aimed at the best possible outcome. Early detection remains the key to successful treatment.
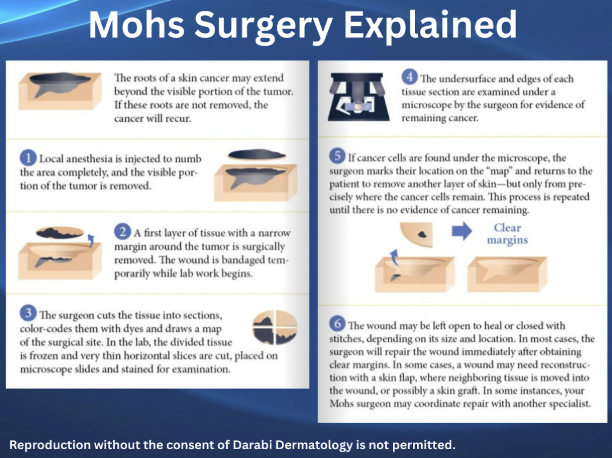
Mohs micrographic surgery is a specialized procedure that takes a precise, methodical, and conservative approach in order to fully remove your skin cancer. Dr. Darabi will be performing your Mohs surgery. Dr. Darabi is a uniquely specialized surgeon who is not only trained and board-certified in Dermatology and Mohs Surgery but is also a board-certified Dermatopatholgist. A Dermatopathologist is a doctor trained and qualified to examine and diagnose skin samples under the microscope. Mohs surgery is the only procedure where the same surgeon removing your skin cancer is also the pathologist looking at your tissue under the microscope. Mohs surgery is also the only skin cancer procedure where 100% of the tissue margins are examined under the microscope, ensuring complete removal of your skin cancer, and offering you the highest cure rate (98-99%) of all methods to remove skin cancer, while your healthy tissue is spared.
On the day of your surgery a nurse will bring you to one of our procedure rooms, any questions that you have will be answered, after you consent your skin cancer will be identified and marked, and then a nurse will use local anesthetic to numb the area. Dr. Darabi will start by removing just the visible skin cancer. This is what is called the 1st stage. The nurse will then place a bandage over your surgical wound and you may remain in our waiting area while your tissue is examined by Dr. Darabi under the microscope. If any skin cancer is seen in the margins of your removed tissue an additional stage will be taken, but only from the areas still affected by cancer. This process is repeated until your skin cancer is gone and you should plan on spending 4-6 hours with us. Skin cancers can be larger than they appear and have microscopic extensions in the skin that can only be appreciated microscopically.
In most cases, after your skin cancer has been fully removed your wound will either heal naturally on its own, or it will be sutured. The choice of self healing or suturing the wound depends on size, location and elasticity of the skin. If your skin cancer was very large, it may need to be reconstructed by a different specialist on a later date. You will have a scar where your skin cancer was removed. However, Mohs surgery takes a conservative approach and is designed to minimize wound sizes and therefore size of scars.
Mohs surgery is performed with local anesthetic. You will be awake. It is OKAY for you to eat and drink like normal, and you are encouraged to do so. If you prefer, arrange someone to drive you to and from your surgery but patients routinely drive themselves to their appointments. If your surgery is around the eye you will have a large bandage protecting your surgical area which may impair your ability to drive. In such cases we recommend a driver.
You must also take your medications normally, especially if you take blood pressure or blood thinning medications, unless you were told to do so otherwise. Bring your medications with you if you need to take them throughout the day.
Mohs surgery takes several hours as the removed tissue needs to be processed in the Mohs lab and microscopically examined by the Mohs surgeon. This process typically takes 1-1.5 hrs and may be repeated several times until the cancer has been completely removed. You may spend the entire day with us. We recommend you don’t make any other appointment on the day of your Mohs surgery. Wear comfortable clothes and dress in layers, bring a snack, bottled water and something to occupy your time, such as work, an electronic device or a book to read.
Before a skin excision, patients should eat normally, take their usual medications (unless advised otherwise). On the day of the procedure, wear comfortable clothing and be prepared to rest the affected area afterward.
During the excision, the area is numbed with local anesthetic, and the dermatologist surgically removes the lesion along with a small margin of healthy skin. The wound is then closed with stitches and covered with a sterile dressing.
After the procedure, patients are instructed to keep the area clean, apply Vaseline and a fresh bandage daily, and avoid strenuous activity or stretching the area for 1–2 weeks, depending on the location. Stitches are usually removed in 7–14 days. Our team provides detailed aftercare instructions to ensure proper healing and minimize scarring.